What Are Moisture Lesions?
Also known as Moisture Associated Skin Damage (MASD), there are many terms used to describe moisture-induced skin damage. Moisture lesions can be defined as inflammation or skin erosion caused by prolonged exposure to any type of source of moisture. For example, urine, stool, sweat, wound drainage, saliva or mucus, etc. These lesions can occur in any age group but people with older age are more prone to Moisture Associated Skin Damage. It generally occurs on the buttocks, groins, inner thighs, natal cleft, and skin folds, etc.
Another complicating factor that can lead to mere moisture exposure to the skin includes mechanical factors (friction), chemical factors (irritants contained in the moisture source), or microbial factors (microorganisms). In simple words, the long-term exposure of the skin to moisture leads to moisture lesions. It can be harmful and can cause extensive skin breakdown. To suffer from a moisture-associated skin condition, skin must be in contact with the moisture. It is also known as Perineal dermatitis, diaper rash, incontinence-associated dermatitis, or moisture-associated skin damage, etc.
Pressure Ulcer Vs Moisture Lesions
Patients often get confused between pressure ulcers and moisture lesions due to the presence of moisture that may be the result of incontinence of urine and/or faeces.
Here Are Some Of The Main Key Points Of Differences Between Pressure Ulcer And Moisture Lesions:
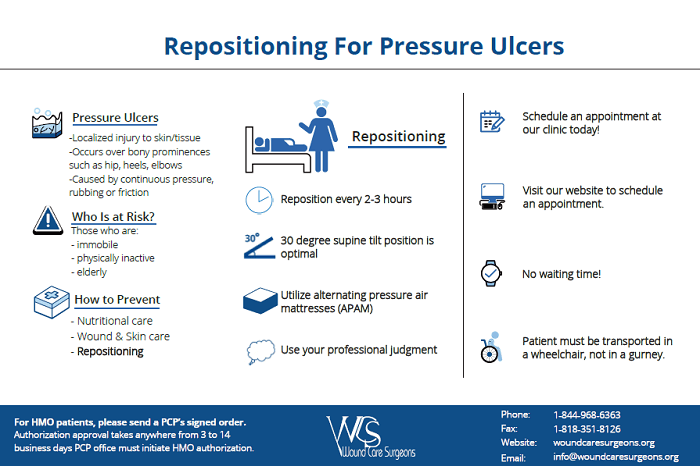
1. Cause - Pressure ulcer occurs due to the prolonged pressure or shear to the particular part of the body while in moisture lesions, there may be desiccation and loose skin.
2. Shape - Pressure ulcers are circular wounds with a regular shape limited to a single spot while moisture lesions can be different superficial spots.
3. Necrosis - It can be present in the pressure ulcers while not in moisture lesions.
4. Color - Red skin or black necrotic tissue are likely to be a pressure ulcer while pink or white skin surrounding a wound is likely to be maceration due to the moisture.
Prevention And Treatment Of Moisture Lesions
On-time assessment and management of continence issues are one of the best ways to prevent moisture lesions from occurring. Here are the following precautions recommended by Moisture Lesions Wound Care that can help reduce the risk of developing periwound moisture-associated dermatitis in at-risk patients. Let’s have a look:
1. Keep an eye on the wound area daily for any type of changes in skin condition.
2. After every occurrence of incontinence, wash your skin using water and emollients. Keep in mind not to use soap.
3. After washing, you need to ensure that the skin is thoroughly dried.
4. Use moisturizers after washing and drying the wound. Make sure that there is antimicrobial content included.
5. Use a barrier protectant film or cream like antifungal or antimicrobial creams.
6. You can use body-worn pads to protect the skin.
The first step to treat the periwound moisture-associated skin damage is managing the excessive exudate. These precautions can help decrease the risks of developing intertriginous dermatitis in at-risk patients or the patients can avail of guidance or wound care services from Wound Care Experts. The staff of qualified and experienced doctors visit your home, evaluate the wound, and generate a customized treatment best fits to wound healing.